Up to 91% of those with autism also have gastrointestinal disorders as a comorbidity with autism. If you want an optimal outcome for your child, be sure to address any GI problems they have.
Now, the problem with GI disorders is that those with autism use behavior to communicate their GI symptoms, which is very different than typical children. GI pain in someone with autism can we expressed as behavior such as:
- aggressive behavior
- self-injurious behavior
- chewing on their clothes
- sobbing
- pacing
- jumping up and down
- much, much more
These behaviors are not “just autism.”
Autism Comorbidities
Co-morbidity is defined as a simultaneous presence of two chronic diseases or conditions in a patient, and this commonly happens with autism.
There’s evidence of an association between various pathophysiological abnormalities and autism, but the exact relationship has not been defined yet.
However, treatments for some of the comorbidities are well known. Therefore, there is no reason for your child to suffer which certain comorbidities. There are many things that are technically a comorbidity and it’s not part of autism.
Those comorbidities can be treated many times very easily. So please, when you’re looking at your child, and you’re trying to get towards that optimal outcome, there’s autism to be treated, and then there are comorbidities to be treated. Two separate things, and it’s really important to know what comorbidities your child has in addition to autism.
Here’s a list of comorbidities -these are very common:
- seizure and epilepsy
- Neurotransmitter disorders
- sleep disorders
- metabolic disorders (folate, cobalamin, tetrahydrobiopterin, carnitine, redox, and mitochondrial)
- immune disorders
- gastrointestinal disorders
GI Disorders And Autism
Up to 91% of those with autism also have a range of GI symptoms. So GI disorders are one of the absolute most common comorbidities to have with autism.
There’s a lot of behaviors that are wrongly interpreted to be autism. Behaviors, including problem behaviors, may be markers of abdominal pain or GI discomfort in those with autism. So a lot of times of those with autism are just written off as, Oh, that’s just part of autism. But they are not. They are absolutely not.
This came from a research article, a highly respected research article. And this is a table from that research article.
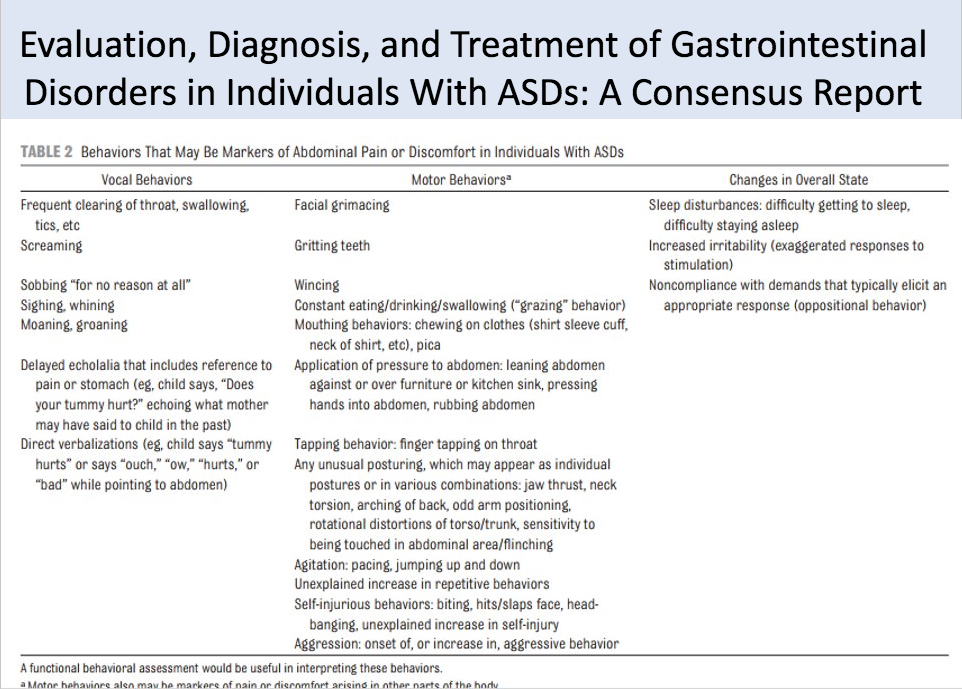
The lead author on this is one of the top gastrointestinal specialists specializing in autism in the world, and the coauthors on this article world-renowned as well. So these are the absolute experts in autism and gastrointestinal disorders.
And I pulled out the table above and it’s table two from that research article, and it says behaviors that may be markers of abdominal pain or discomfort in individuals with autism.
So I really want to focus on this because many of these behaviors are just written off as part of autism and they’re not so vocal behaviors, frequent clearing of throat, swallowing different ticks, screaming that sobbing, quote unquote, for no reason at all. And quote, there is a reason. Please don’t think your child is crying for no reason at all.
Or that sobbing is just part of autism. It’s not. Sighing and whining and moaning and groaning delayed echolalia – and that includes reference to pain or stomach. So if your child keeps repeating back, the question that you ask them, does your tummy hurt? They’re trying to indicate that their tummy hurts.
You could have direct verbalizations. So the child says, tummy, tummy hurts ouch. If your child is nonverbal, many times they’ll either take your hands to their stomach or they’ll just hold their stomach, they will try and get your attention towards their stomach area.
So motor behaviors, things like facial grimacing, and these are again, things that those who are nonverbal or verbal can do.
And these are behaviors that may be the markers of abdominal pain or discomfort:
- facial grimacing
- gritting of the teeth
- wincing
- constant eating, drinking, swallowing (grazing behavior)
- mouthing behaviors
- chewing on clothes
- application of pressure to the abdominal (posturing)
- tapping behaviors like finger tapping on the throat
- agitation (pacing, jumping up and down
- unexplained increase in repetitive behaviros
- self-injurious behaviors (biting, slapping, headbanging)
Posturing can be – if you’ve seen your child like hanging off the couch by their stomach, they’re really trying to put pressure to relieve the pain. They can have tapping behaviors, so finger tapping on the throat posturing so that they might actually twist their posture in a particular way that might be agitated.
So pacing, jumping up and down. Right? We have many children with autism who jump up and down. That’s not necessarily to be written off as, Oh, that’s part of autism. It’s certainly can be agitation that is significant of abdominal pain or discomfort. There’s also an unexplained increase in repetitive behaviors, self-injurious behaviors, including biting, slapping, headbanging.
All of those behaviors that when we see our children do it, it’s nerve-wracking. So those self-injurious and aggressive behaviors, many of those times, it’s actually because your child’s in pain, not because it’s just autism.
Changes in overall state sleep disturbances. So difficulty getting to sleep, difficulty staying asleep, increased irritability, and noncompliance with demands that typically elicit and appropriate response.
If you start thinking that your child has ODD (oppositional defiant disorder), it really might be that they’re in pain and they are having GI disorders.
These are behaviors that world-renown gastrointestinal specialists who also specialize in autism have set forth as behaviors that may be markers of abdominal pain or discomfort in those with autism.
If your child’s showing any of these behaviors, you should definitely follow up with a functional medicine doctor who also specializes in autism.
Microbiota And Autism
Many studies show that the gut microbiota is atypical and those with autism, and there are so many studies showing this, so they show there’s:
- decreased species diversity
- over-representation of certain species
GI Treatments
I’m sure everyone’s wondering, okay, that list of behaviors is pretty big. So what do I do? What kind of treatments are there out there? Children with autism deserve the same standard of care, addressing GI symptoms as those without autism.
Unfortunately, the reality is those behaviors that our children’s show, which is actually their way of saying they’re having GI problems, they’re written off as just, oh, that’s part of autism, and it’s not. It’s a comorbidity. It’s really important to understand those two, especially if you’re going for an optimal outcome. Children with autism might present with behavioral symptoms rather than more typical GI symptoms. So this is why your child’s behavior matters. It’s not just autism. Please do not think that.
Diet is a common and effective way to treat GI symptoms. There are many studies that have been trying to analyze the effectiveness of diet, and those studies have been inconsistent, and mainly it’s due to clinical trial design. Each diet that’s out there specifically targets certain symptoms.
So if you want to have success for your child on a special diet, it is absolutely vital to match the diet to all symptoms. You could pick a diet, let’s say, a gluten-free, casein-free, soy-free, right?
You want to spend all this time, energy, effort, and money getting your child on a gluten-free, casein-free, soy-free diet and the symptom, let’s say that is the main driver for that is their ADHD or anxiety type behaviors -either one of those symptoms. You should know that the gluten-free casein-free, soy-free diet, does not address anxiety or ADHD type behaviors.
So this is why when you pick a special diet for your child, you really have to understand what symptoms that diet addresses so that you pick the right diet.
Digestive Enzymes And Autism
Some children with autism have shown to have deficient levels of digestive enzymes to properly digest their food. And this is where some of their pain and discomfort and then further down the line, their problematic behaviors come from.
There was a three-month double-blind placebo-controlled clinical trial of 101 children with autism. And that report found significant improvements in autistic behaviors, emotional response in GI symptoms with digestive enzyme treatment within those three months.
The authors of this research actually came from Egypt, the United States, Saudi Arabia, and Norway. So this is really exciting in the time of autism research, so many countries have researchers working on problems like this and working together.
Because the researchers know that improvements and optimal outcomes can be had, it just takes a lot of understanding -the comorbidities. There are children all over the world having optimal outcomes from autism, meaning they lose their diagnosis, they heal completely. They go on to live lives without needing all this additional support.
It’s really great to see scientists working together from all over the world. And I love seeing children all over the world get optimal outcomes and completely heal from autism.
Microbiota Treatments
Many use special diets and probiotics to rebalance the microbiota.
An open-label study using probiotics with those with autism reported improvements in concentration and following directions.
In a double-blind placebo-controlled crossover study improvements in stool consistency, autism behaviors, as well as the reduction in Clostridium species were seen.
Rebalancing the microbiota for anyone who has autism is really important. But unfortunately, the reality is that most children with autism are not taking the right probiotic. Rebalancing the microbiota does not mean just taking one bottle of probiotics. It’s a much more systematic approach to rebuilding the microbiota that is an effective way of rebalancing.