Research has shown that somewhere around 80% of those with autism will have difficulty with sleep at some point in their life. We all know when we don’t sleep, the next day is pretty rough. And with each night of not sleeping, the following day gets tougher and tougher and tougher. It becomes hard to function. But what does the research say about why that’s true in autism? How does lack of sleep really affect our children’s brain – Negatively? or Positively?
There is cutting-edge scientific research that gives a good perspective on what happens on the molecular level to our children’s brains when they don’t sleep and how that actually impacts brain function.
If you’ve ever wondered why your child’s autism symptoms increase when they don’t sleep, let me explain Cerebrospinal fluid and autism research. You can watch the video below so that I can show you the cutting-edge science. It’s pretty amazing and explains quite a bit about autism.
Cerebrospinal Fluid, Sleep, and Autism
Cerebral spinal fluid (CSF), often referred to as fluid in the brain, plays a remarkable role in maintaining the health and functionality of the central nervous system. For children, particularly those with autism, understanding the significance of CSF becomes even more crucial.
When we talk about CSF, we’re not just discussing fluid in the brain; we’re diving into the intricate mechanism that safeguards the brain’s well-being. This clear, watery fluid not only acts as a cushion, protecting the brain from physical shocks, but it also serves as a vehicle for waste removal. One component of the brain where CSF’s influence is gaining recognition is the claustrum. While not as well-known as some brain structures, the claustrum is now being examined for its potential involvement in consciousness and sensory integration. Recent studies have suggested that CSF might be present in the claustrum, hinting at a connection between this mysterious region and the fluid’s vital functions.
Understanding how CSF interacts with the claustrum fluid is a fascinating area of biological science. It underscores the intricate interplay within the brain and how disruptions in this system could have implications for various neurological conditions, including autism. So, when we advocate for healthy sleep patterns in children, we’re not just promoting a good night’s rest; we’re nurturing a process that involves the dynamic balance of cerebral spinal fluid, potentially influencing the well-being of our young ones, especially those on the autism spectrum.
Cerebrospinal fluid’s purpose – what does it do?
There are two primary functions of cerebrospinal fluid, and they are the delivery of growth factors and other molecules needed for healthy neural growth. Think nourishment. There’s the delivery of nourishment that the brain needs. And then here’s a direct quote:
“Cleaning of the brain by removing neurotoxins and metabolic waste byproducts of neuronal function.”
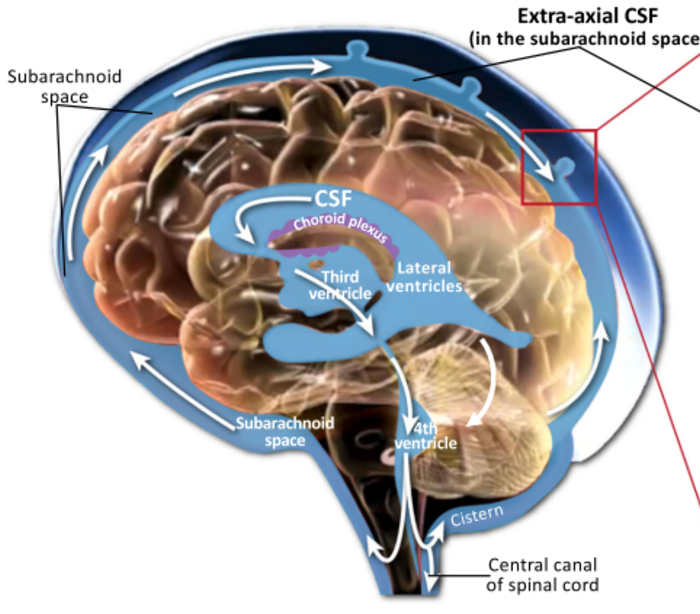
A detailed diagram of cerebrospinal fluid below shows how fluid moves in the brain:
Understanding the intricate journey of cerebrospinal fluid (CSF) within our bodies offers profound insights, especially when considering children with autism. The path of cerebrospinal fluid, a clear, colorless body fluid found in the brain and spinal cord, is vital for brain health. It is secreted by the choroid plexus, a tissue found in the ventricles of the brain, and plays a crucial role in cushioning the brain and removing metabolic waste.
Children, especially those with autism, need enough sleep for the lymphatic system to work well and remove toxins from the brain with the help of CSF. The occurrence of extra fluid in the brain, known medically as hydrocephalus, can be a concern in some cases and is closely monitored. What produces cerebrospinal fluid, and its regulation, is key to understanding various neurological conditions. CSF fluid’s movement and turnover are significantly higher during sleep, underlining the importance of good sleep hygiene in children.
Unfortunately, lately in the mainstream media, detox has become just this kind of like hashtag. And I just want to state that detoxing is a legitimate biological process. I have another video that goes into the basics of CSF, and here it is. But just very quickly, to summarize, studies show that there is an increase in CSF fluid as measured with an MRI in infants that later go on to develop Autism.
There’s too much CSF in the brains of those infants that later go on to develop autism. This is not for every person with autism. These are studies that are starting to show this. Increased CSS volume means that CFF is either stagnant or there is reduced circulation. One of those, or sometimes it could be both.
CSF Stagnation
Let’s get into stagnation a little bit. There’s a direct quote from the research article:
“Stagnation of CSF leads to the accumulation of neuromodulators in brain tissue that may alter the extracellular environment of neurons and impact their growth and function.”
Basically, too much of a good thing is not a good thing. When absorption and production is unbalanced, then the concentration of those “good things” is disrupted and it could actually alter brain development.
CSF & Neuroinflammation
Let’s look at neuroinflammation.
“The primary function of continuous CSF outflow is the removal of inflammatory byproducts of brain metabolism such as amyloid beta and tau protein.”
That’s a direct quote from the research article. And yes, if you’re thinking that kind of sounds like Alzheimer’s disease, you are correct. There is certainly overlap in this aspect of science. So let’s go through the three ways that the brain does this detoxification and this CSF clearance.
First: in the mature brain: Reabsorption into arachnoid granulations, which are these one-way valves that drain into the sinuses. The thing is that these do not develop until after 18 months of life. So during infancy, these typically are not functioning.
Clearance number two: The flow of fluid is facilitated by Astroglial-aquaporin-4, (AQP4) channels, and thus is named the Glymphatic system.
That’s Glial and Lymphatic. The Glymphatic system is real and not just a buzzword. It is on the recent side of being discovered and starting to be fully understood. That’s why if you ask certain doctors about this, they might just not know.
Clearance number three: The Meningeal lymphatic system provides another clearance route for CSF and inflammatory proteins. The thing with this is it was only discovered in 2015. Again, depending on the doctor you talk to, how well-read they are, when they got their degree, all of these things, they might not even know about this particular system. And these Meningeal lymphatic vessels provide a direct path between the nervous and the immune system for the immune cells to exit the CNS. You can see how the body is all connected, the nervous system and the immune system. We’re only really getting to discover the connection in 2015. There is so much that can be going on in one aspect of a person’s body that really impacts many others. And because these clearance systems act together, right, all three, to drive amyloid beta from the brain and other neurotoxins, any alteration in the given systems could contribute to the accumulation of neuroinflammation.
We don’t want any of these clearances to be blocked, right? We want the brain to be able to produce enough for there to be adequate flow and for there to be clearance. All of that is important to have an optimally functioning brain.
Sleep and CSF
Alright, let’s get into sleep. During natural sleep, there is an increase in CSF as compared to when you’re awake. And this detoxing, this exchange of CSF is accelerated during sleep. Sleep is really important. If you’ve ever realized when you didn’t get a good enough sleep the next day, your brain is just a little bit off, this could be one of the reasons. Were you able to detox enough? Maybe not. Then that might actually impact your next day. This increased flow of CSF during normal sleep facilitates the increased clearance of amyloid beta and other neurotoxins, which is continually secreted by neurons and needs to be continually removed by the efficient flow of CSF. You need this detoxing to happen every night. Disrupted sleep hinders the flow of CSF and its ability to clear not just amyloid beta, but any other neurotoxin that your brain has been exposed to during the day.
Disrupted sleep hinders this process. Unfortunately, sleep problems are experienced by the majority of those with autism. Sleep problems, yes, you’re grouchy the next day, and you’re irritable, and you might be eating more, and there’s a lot that, behavior-wise, you could see, okay, things are different. But on the molecular level, this is one of the things that is happening when your child is not getting enough sleep. Their brains literally are not able to do the normal detoxification that goes on during the night.
A study showed that worse sleep problems in preschool children with autism were associated with greater CSF volume. And now that’s pretty profound. The more CSF volume that has been accumulating in the brain, the worse the sleep problems. And you can see how that cycle will just continue. Behaviors will be worse, and then sleep will be worse, and detoxification will be worse, and you’re going in the wrong direction. You want sleep to be high-quality sleep because it’s so impactful.
Next Steps
Unfortunately, in this paper, there are no conclusions, just the next steps. This is cutting-edge research, and I really wanted to show you how the field evolves and how doctors are really learning so much more about our bodies.
So their conclusion, or lack thereof, or we call this next steps in order to validate the CSF as a potential stratification biomarker. Right? Because you might be thinking like, well, why don’t we just start to study our children when they’re at six months, when we first start to have concerns? The field doesn’t evolve like that. There has to be different steps, right?
- A. Is to determine its specificity. Compare it to other neurodevelopmental disorders.
- B. Then you would want to elucidate the underlying biology. You use animal models. Look at genetic associations. You can see we’re talking years here, right? Using animal models, that’s at least two years. And that would be one model. You need multiple of these before this could really be called a biomarker.
- C. You would also test potential mechanisms using experimental approaches, such as those established by the studies described above. Blah, blah, blah, blah, blah. Right? So there’s got to be a lot more science that is done before the scientific community and the medical community can say, okay, CSF volume is now a biomarker in these particular times. They’ll probably have a cut-off for what would be considered extra CSF volume. All of these studies have to go on before the field will change.
There’s a lot. There’s so much that goes into classifying something as a biomarker. And now you might be sitting there like, okay, why are you telling me all this stuff if it is not going to help me at this moment.
The thing is, you don’t have to wait 20-30 years to get an answer.
What About Now?
Make sure your child is getting enough quality sleep.
Absolutely one of the first things, when I’m working with clients, that’s one of the first things I ask about. That’s one of the first metrics that I have. Once we get the child sleeping well, oh, goodness! Life becomes so much better for the parent and the child. But that becomes one of the metrics that once the child is sleeping well, I always tell the parents, if your child has disrupted sleep, like, two nights in a week, you got to let me know because something is going on. It’s an early indicator that I’ve experienced saying something is not right.
So what can you do? Ask your doctor this question: “What is preventing my child from getting quality sleep?”
If the doctor says, “I don’t know.” Find another doctor.
If the doctor tells you, okay, let’s look at this certain aspect, and it helps 50%. And you ask them again, what is preventing my child from getting quality sleep? And they don’t know. Find a new doctor. Right. You want to keep looking for someone who can help you until this question is answered.
Your child needs adequate sleep every night for so many reasons, and it’s absolutely important. And if you have done an MRI already, some parents have, and some haven’t. If you haven’t, do not stress about it. If you have done an MRI already, you can ask the radiologist about the formation of the ventricles. You can ask about the CSF flow. You can ask some structural-related questions just so that you yourself get a better idea. And you might be working with a doctor who is very familiar with these research studies, and that would be absolutely excellent. You don’t have to wait 30 years for the field to evolve. You can start taking really logical steps in improving your child’s health.
And there’s no need to quote studies. You don’t have to send an email to the radiologist with links to PubMed and all these kinds of things.
I find that simple questions, simple but profound questions are the best way to really start that dialogue and build a partnership with your doctor. You can ask the radiologist, how is the brain structure formed? Is there anything that’s formed abnormally? That’s a great question. To get the conversation going, you can ask about the ventricles. You can ask about anything else structure-wise, and it will start getting the conversation going.
Reference
And here is the reference that I’ve used: