Does your child have gut dysbiosis?
Has improving their gut improved other symptoms as well?
Is there some science to back that?
Welcome to my video series on microglia.
In this post, we will explore the microbiota and microglia. There is now compelling scientific data suggesting that the intestinal microbiota can play a causative role in driving the behavioral changes associated with autism. That is a direct quote from a scientific paper.
Gut dysbiosis is common in those with autism. But interesting therapies targeting the microbiome can markedly improve or completely remediate behavioral symptoms. The interplay between the gut Microbiota and the brain cells called microglia is important to understand. Come learn about the microglia so that you have up-to-date information. You can watch the video above to see my slides and know what I’m talking about.
Microglia, Microbiota and Autism
Alright, just a warning here. This is an advanced topic. This information is very useful after beginning steps have been taken in the autism journey, there are many beginner steps to take. And doing advanced steps early usually doesn’t make the impact that one might be seeking. You can certainly watch this video and learn what could be possible in the future. But if you haven’t done the basic steps, focus on those.
Microglia play several fundamental roles in orchestrating brain development and homeostasis. If you want to learn some of the basics about microglia and autism, I do have a video.
About the basics of microglia: the one point to really remember about microglia is that they are highly sensitive to environmental cues.
Autism and the Gut
Research studies have shown that the intestinal Microbiota can play a causative role in driving the behavioral changes associated with autism. If you or your child has had autism for a while, I’m sure this is nothing new, but I want to make sure we cover some of the foundations.
Not only is intestinal dysbiosis commonly reported in those with autism, but therapies targeting the microbiome can markedly alleviate behavioral symptoms.
This is why probiotics have certainly become quite popular, but it’s not as simple as just taking a probiotic. There’s a lot of synergy involved in optimal health.
Let’s understand the reciprocal interactions between microglia and intestinal microbes that could play a crucial role in autism, and I say reciprocal. So there’s two-way communication between microglia and intestinal Microbiota.
Microglia and Autism
Several studies show that autistic individuals have ongoing neuroinflammatory health issues characterized by microglia activation in certain discrete regions of the brain.
So what that says is not everyone with autism has issues with microglia and not everyone with autism who have issues with microglia would have it in the same region of the brain. This is where some people say autism can get really complex. It’s because it’s not homogeneous, everyone doesn’t experience neuroinflammation the same way. That really shouldn’t come much of a surprise, but anyway.
Some dispute the significance of this and suggest that microglia may be intrinsically dysfunctional. So there’s controversy. And as scientific theories develop, there’s always controversy. That’s how they develop into the best theory possible. The question to ask yourself and then a well-trained doctor is does my child have neuroinflammation?
If they don’t, right, and you want to measure it, you want to work with a doctor who can actually answer that question with truth and with lab results, then this is not something to be concerned about.
But if your child does have neuroinflammation, as many do, then this is where you want to start getting more and more granular.
Microglia and Autism
It’s in the early stages of understanding. There’s not a full consensus yet. There’s still debate, there are still different research studies going on to really understand this topic. In 2005, that’s when the first scientific article was published showing an inflammatory phenotype. That just means you could see it physically in the postmortem brains of those with autism. So that’s only in 2005. In that research, it showed that increased microglia activation was present. It was also present with increased inflammatory markers in both the brain and the cerebral spinal fluid.
I do have two videos on cerebral spinal fluid and autism research. The links have been provided if you want to learn about cerebral spinal fluid. Again, that is cutting-edge research. All that I’m talking about here is new research within the past decade or so.
Neuroinflammation is Real
I know on social media and Facebook, and there are so many just buzzwords and I don’t know, people use words that I don’t think maybe they even know what it is. But neuroinflammation is real. Other research studies have reported increased neuroinflammation in postmortem brain tissue and cerebral spinal fluid of children with autism, suggesting a heightened immune response with associated localized brain inflammation. So once again, neuroinflammation is real. And the characterization the scientists were able to do is they looked at TNF alpha and several different interleukins. So it’s not just this broad blanket statement, oh, there’s neuroinflammation. No, you can actually quantify the neuroinflammation if you’re looking at these different markers.
Autism and the Gut
GI dysfunction is one of the most prominent comorbidities in those with autism. And that’s things like abdominal discomfort, irritated bowel syndrome, chronic diarrhea and or constipation. The list can go on and on. Variations in the composition and diversity of the gut Microbiota in those with autism have been observed to be different compared to neurotypical controls. So we know the gut composition in those with autism is different. I don’t believe this is disputed anymore in the scientific community.
Microglia and Autism: microglia are highly sensitive to environmental changes, right? That was the one thing to remember in this video about microglia. microglia are highly sensitive to environmental changes, not just locally in the brain, but throughout the body. The body is connected on the most basic level. Microglia are readily activated in response to systemic inflammation. So if there’s inflammation going on somewhere else in the body and the microglia can sense it, they’re going to be activated if the cause is great enough. So if this systemic inflammation is ongoing and let’s say it’s increasing, it can actually trigger the activation of microglia in the brain.
This is a really important point to remember that if the systemic inflammation is great enough, then that can trigger the activation of microglia in the brain, while the gut Microbiota will not induce systemic inflammation if a person has a healthy, optimally functioning gut. It has been well-documented that autism is associated with barrier defects in the GI tract. This is what’s often referred to as a leaky gut. Scientists hate the term, leaky gut, but that’s the buzzword in mainstream media. And those with autism also have impaired blood-brain-barrier integrity.
So if someone has a healthy, optimally functioning gut, and let’s say there’s some type of inflammation within the gut, typically the microglia would not be activated in that instance because their gut is functioning and it will contain it.
However, those with autism often have intestinal permeability issues. That’s the way scientists like to say leaky gut as well as the impaired blood-brain barrier. And so the inflammation that is going on in the gut can actually spread outside the gut and then that is what can trigger the microglia to activate.
Here’s a quote from the research article:
“Thus, it is possible that inappropriate trafficking of bacterial cell wall components through the intestinal barrier to the central nervous system through a permissive blood-brain barrier could contribute to abnormal microglia activation and associated neurological symptoms.”
Microglia can sense peripheral changes in more subtle ways, and it is becoming increasingly apparent that they respond to changes in the gut’s Microbiotatic composition. Even though the gut is quite far away from the brain, gut disruptions can be sensed by brain cells. The gut microbiota can influence both microglia maturation and activation.
Here’s a figure from that research article in case someone wanted to have a little more visual learning.
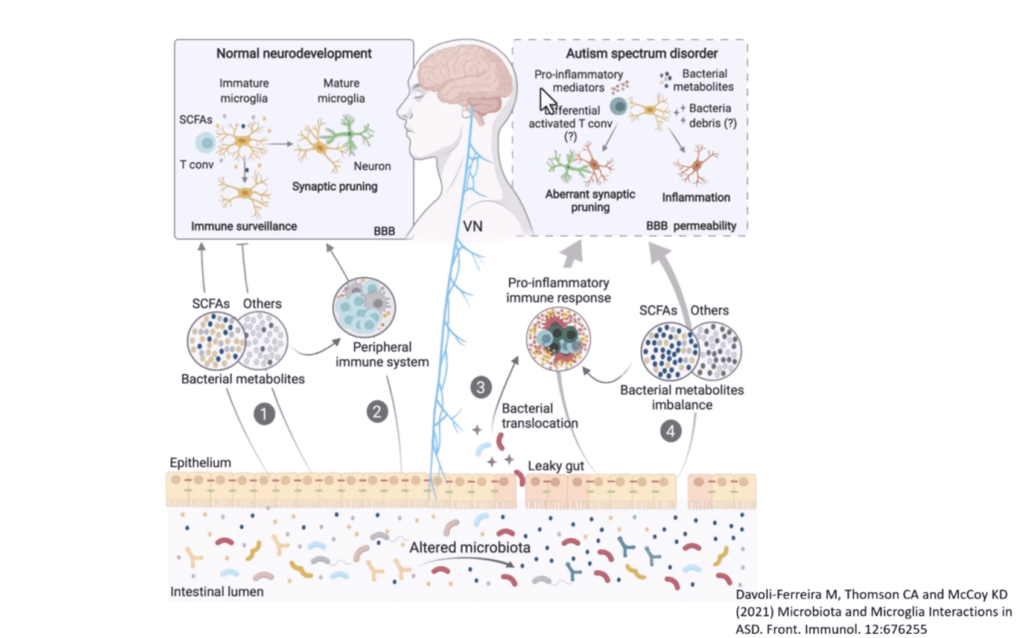
I don’t know about normal neurodevelopment, I would say an optimally functioning gut. And this is over here in the autism spectrum. And so what could potentially be happening? And again, this is the reference.
Conclusion
“Although it is yet to be fully established, a causal relationship between immune dysfunction dysbiosis and the barrier defects associated with autism patients seems likely. And we proposed this as a major factor in the maintenance of neurological dysfunction in autism.”
And here is the reference: