Ever wonder why camel milk has become popular?
Why do some parents insist that camel milk helped their child with autism? Camel milk in the US is exotic. However, parents have been spending quite a bit of money to buy it. In other parts of the world, camel milk is common and those parents are also buying it for their children with autism. Why?
Is there actually a difference between cow’s milk and camel milk?
Why would one be preferred over the other?
And here’s the most important question: What does the science say?
There was a publication that came out in 2022 that explored the effects of camel milk on children with autism as measured with blood tests. Let me get my slides so you can see what I’m talking about.
Science of Camel Milk in Autism
Nutrition strongly influences many chronic inflammatory diseases, with food metabolism being closely linked to inflammatory processes. Inflammation could be a result of a rejection of a food substance due to our body’s immune response and the interplay between nutrition, immunity, and inflammation has become a hot topic for research and an easy aspect for parents to focus on first in improving their child’s health. This is the reason why diet and autism is such a huge topic because diet really does influence so much of what goes on in our body.
Cow milk
Milk is the primary dairy product at the beginning of many children’s lives. Consumption of conventional cow milk is associated with small intestine inflammation. Conventional cow milk releases beta-casomorphin, which increases opioid activity in the GI system. Milk protein, specifically the beta-casein is associated with increased intestinal permeability, otherwise known as leaky gut, and also potentially leads to neurological disorders, including autism.
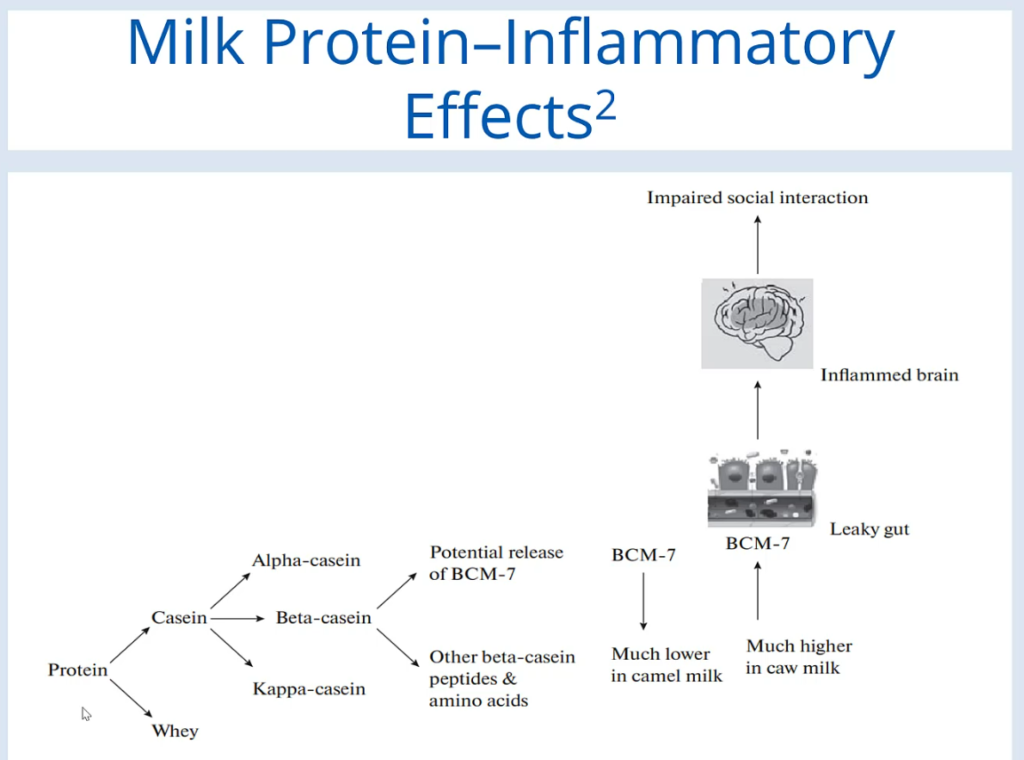
Let’s get into the inflammatory effects of milk. As you can see here, this is a figure that’s going to describe the milk protein inflammatory effects. This is taken from a publication about camel milk in 2022. You start out with the protein and you have casein and whey.
We’ll focus on the casein and you have a variety of different types of casein. They’re focusing on the beta-casein and there’s a potential release of BCM-7. And this particular protein, BCM-7, is much lower in camel milk. It’s much higher in cow milk. BCM-7 is much higher in cow milk and BCM 7 contributes to increased intestinal permeability or leaky gut, which then can also influence an inflamed brain and impaired social interaction. That’s the figure from this particular research article on camel milk and autism.
Benefits of Camel Milk
Why is camel milk such a hot topic? Isn’t milk just milk? No, it’s not.
Camel milk has become increasingly popular because it has a lower concentration of A1-Beta Casein. Additionally, camel milk has therapeutic qualities such as antibacterial, antiviral, anti-inflammatory, antidiabetic, and anti-allergenic. Camel milk also has a significantly lower Omega six-Omega three ratios as an anti-inflammatory index.
So that’s 2.12 Vs 13 of the cow milk. And it also contains three times more Vitamin C than cow milk.
Let’s get into the study that was published in 2022 about camel milk and autism.
So the whole purpose was to investigate the therapeutic potential of raw and boiled camel milk in reducing neuroinflammation. And then we’re going to compare the effects of raw and boiled camel milk consumption versus cow milk consumption.
The sample size was 64 children with autism. The age was two to twelve years old. The duration was two weeks. That is a relatively short duration. The pro-inflammatory biomarker used to measure autism severity was chosen to be TNF Alpha. And how these scientists measured behavioral changes was using the Childhood Autism Rating Scale and the Social Responsiveness Scale. They also measured gastrointestinal symptoms.
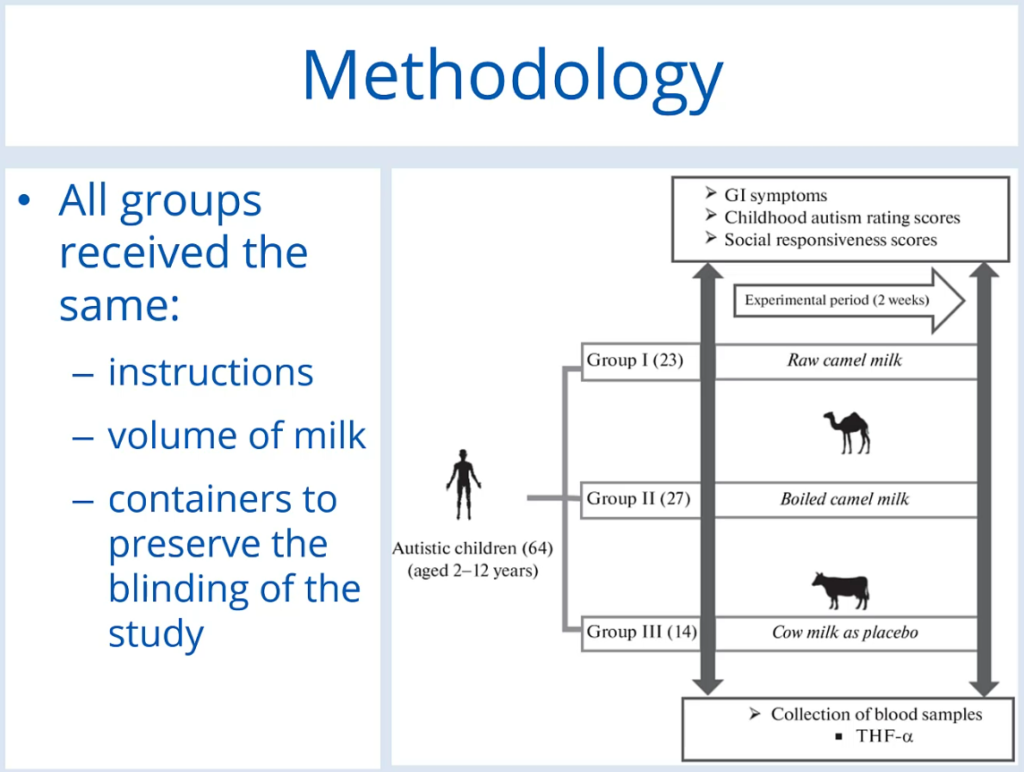
Here’s the methodology. All groups receive the same instructions, the volume of milk, and containers to preserve the blinding of the study. And you can see how there were 64 children with autism and they were broken into three groups. 23 consumed the raw camel milk, 27 consumed the boiled camel milk, and 14 consumed the cow milk, which was (they’re calling) a placebo. And these wonderful children were able to get blood draws and that is what they were measuring TNF-Alpha.
TNF Alpha results
It showed that there is actually a reduction in inflammation consuming camel milk, whether it was boiled or raw.
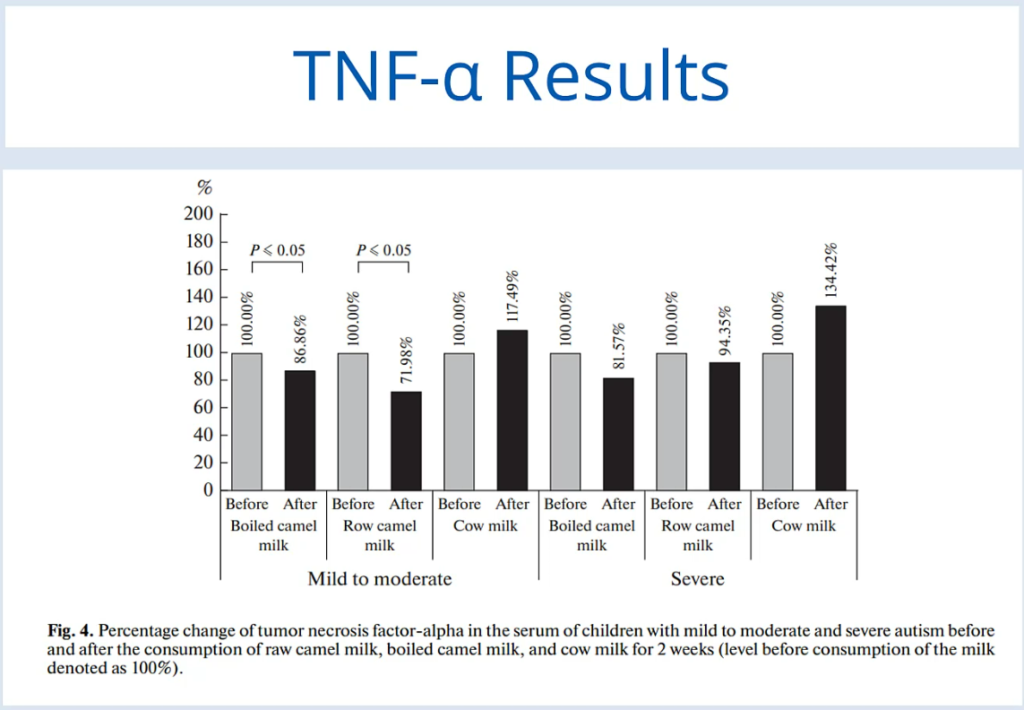
You can see here that there is an actual decrease in inflammation as measured by TNF Alpha results from blood tests. For the cow milk, you can see there’s actually an increase in inflammation as measured by TNF Alpha. This was in the group of those with autism that was classified as mild to moderate. They also broke it out for severe autism. And again boiled camel milk – you can see a reduction in neuroinflammation as measured by TNF Alpha. The raw camel milk, not as much of a change, but again a little bit – 6%. And then the cow milk again and you could see how much of an increase in neuroinflammation there is here with the cow’s milk consumption after two weeks.
Here are some results about the gastrointestinal symptoms. You can just see across the board that GI symptoms did decrease with the camel milk.
Conclusions
Camel milk has therapeutic potential due to its antiviral, antifungal, antibacterial, antioxidant, and anti-inflammatory effects. These effects are mainly due to two active ingredients, Lactoferrin, and immunoglobulins. Lactoferrin in camel milk specifically inhibits the growth of microorganisms known to be highly abundant in the feces of patients with autism compared with those of healthy individuals.
It seems camel milk is addressing dysbiosis in the gut of those with autism. Lactoferrin is having an impact in the microbiota of someone with autism. Results demonstrate a significant decrease in TNF Alpha as a marker of inflammation in the serum of children with autism after consuming raw or boiled camel milk for two weeks.
That was the study’s conclusion and that is why camel milk is starting to increase in popularity in parts of the world where it’s considered exotic because it has particular health benefits that people want.
Camel milk consumption is accompanied by a much lower number of participants with GI symptoms.
And here are some references: